MDB nedenleri

MDB'nin Nedenleri Nelerdir?
MDB'nin kesin nedeni belirsiz olsa da, aşağıda ayrıntılı olarak tartışılan bir dizi katkıda bulunan genetik ve çevresel faktör tanımlanmıştır.1
Bir meta analiz çalışmasında genetik ve çevresel faktörler aşağıdaki şekilde gösterilmiştir:1
MDB'nin alt tipleri için ek belirtiler ve değerlendirmeler aşağıdakileri içerir:
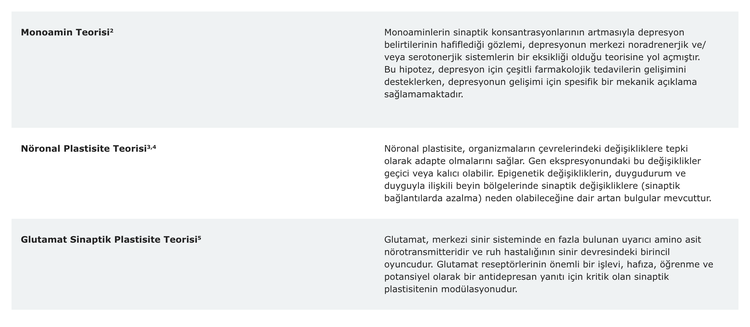
Not: "Sinaptik plastisite", önceden var olan sinapslarda sinaptik iletimin gücü veya etkinliğinin aktiviteye bağlı modifikasyonunu ifade eder.6

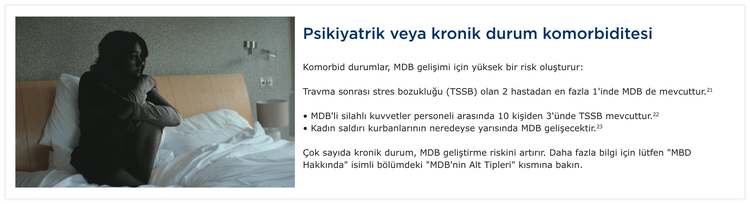
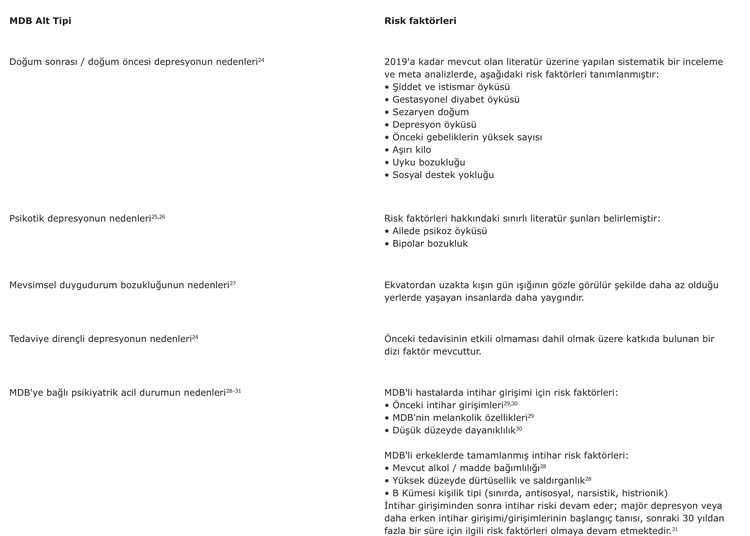
MDB alt tipleri için bazı yaygın risk faktörleri

MDB tedavileri hakkında daha fazla bilgi edinmek için "Tedaviler" isimli sayfayı ziyaret edin.
Kısaltmalar
MDB: Majör Depresif Bozukluk, TSSB: Travma Sonrası Stres Bozukluğu.
Referanslar
[1] Sullivan, P. F., Neale, M. C. & Kendler, K. S. Genetic epidemiology of major depression: review and meta-analysis. Am. J. Psychiatry 157, 1552–1562 (2000).
[2] Hirschfeld, R. M. A. History and evolution of the monoamine hypothesis of depression. J. Clin. Psychiatry 61, 4–6 (2000).
[3] Uchida, S., Yamagata, H., Seki, T. & Watanabe, Y. Epigenetic mechanisms of major depression: Targeting neuronal plasticity. Psychiatry Clin. Neurosci. 72, 212–227 (2018).
[4] Penner-Goeke, S. & Binder, E. B. Epigenetics and depression. Dialogues Clin. Neurosci. (2022).
[5] Murrough, J. W., Abdallah, C. G. & Mathew, S. J. Targeting glutamate signalling in depression: progress and prospects. Nat. Rev. Drug Discov. 16, 472–486 (2017).
[6] Citri, A. & Malenka, R. C. Synaptic plasticity: multiple forms, functions, and mechanisms. Neuropsychopharmacology 33, 18–41 (2008).
[7] Wray, N. R. et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat. Genet. 50, 668–681 (2018).
[8] Kessler, R. C. & Bromet, E. J. The epidemiology of depression across cultures. Annu. Rev. Public Health 34, 119–138 (2013).
[9] Giannelis, A. et al. Examining the association between family status and depression in the UK Biobank. J. Affect. Disord. 279, 585–598 (2021).
[10] Bulloch, A. G., Williams, J. V, Lavorato, D. H. & Patten, S. B. The relationship between major depression and marital disruption is bidirectional. Depress. Anxiety 26, 1172–1177 (2009).
[11] Angst, J. et al. The epidemiology of common mental disorders from age 20 to 50: results from the prospective Zurich cohort Study. Epidemiol. Psychiatr. Sci. 25, 24–32 (2016).
[12] Vandeleur, C. L. et al. Prevalence and correlates of DSM-5 major depressive and related disorders in the community. Psychiatry Res. 250, 50–58 (2017).
[13] Hasin, D. S. et al. Epidemiology of Adult DSM-5 Major Depressive Disorder and Its Specifiers in the United States. JAMA psychiatry 75, 336–346 (2018).
[14] Depression and Other Common Mental Disorders Global Health Estimates.
[15] WHO/Europe | Gender and mental health. www.euro.who.int/en/health-topics/health-determinants/gender/activities/gender-and-non-communicable-diseases/gender-and-mentalhealth.
[16] Widom, C. S., DuMont, K. & Czaja, S. J. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch. Gen. Psychiatry 64, 49–56 (2007).
[17] Lippard, E. T. C. & Nemeroff, C. B. The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am. J. Psychiatry 177, 20–36 (2020).
[18] Benjet, C., Borges, G. & Medina-Mora, M. E. Chronic childhood adversity and onset of psychopathology during three life stages: childhood, adolescence and adulthood. J. Psychiatr. Res. 44, 732–740 (2010).
[19] Humphreys, K. L. et al. Child maltreatment and depression: A meta-analysis of studies using the Childhood Trauma Questionnaire. Child Abuse Negl. 102, 104361 (2020).
[20] Gutiérrez-Rojas, L., Porras-Segovia, A., Dunne, H., Andrade-González, N. & Cervilla, J. A. Prevalence and correlates of major depressive disorder: a systematic review. Rev. Bras. Psiquiatr. 42, 657–672 (2020).
[21] Brady, K. T., Killeen, T. K., Brewerton, T. & Lucerini, S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J. Clin. Psychiatry 61, 22–32 (2000).
[22] Campbell, D. G. et al. Prevalence of depression–PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. J. Gen. Intern. Med. 22, 711–718 (2007).
[23] D’Elia, A. T. D., Juruena, M. F., Coimbra, B. M., Mello, M. F. & Mello, A. F. Posttraumatic stress disorder (PTSD) and depression severity in sexually assaulted women: hypothalamic-pituitaryadrenal (HPA) axis alterations. BMC Psychiatry 21, 1–12 (2021).
[24] Zhao, X. & Zhang, Z. Risk factors for postpartum depression: An evidence-based systematic review of systematic reviews and meta-analyses. Asian J. Psychiatr. 53, 102353 (2020).
[25] Jääskeläinen, E. et al. Epidemiology of psychotic depression - systematic review and meta-analysis. Psychol. Med. 48, 905–918 (2018).
[26] Buoli, M., Caldiroli, A. & Altamura, A. C. Psychotic versus non-psychotic major depressive disorder: a comparative naturalistic study. Asian J. Psychiatr. 6, 333–337 (2013).
[27] Meesters, Y. & Gordijn, M. Seasonal affective disorder, winter type: current insights and treatment options. Psychol. Res. Behav. Manag. (2016).
[28] Dumais, A. et al. Risk factors for suicide completion in major depression: a case-control study of impulsive and aggressive behaviors in men. Am. J. Psychiatry 162, 2116–2124 (2005).
[29] Xin, L.-M. et al. Risk Factors for Recent Suicide Attempts in Major Depressive Disorder Patients in China: Results From a National Study. Front. psychiatry 9, 300 (2018).
[30] Sher, L. Resilience as a focus of suicide research and prevention. Acta Psychiatr. Scand. 140, 169–180 (2019).
[31] Probert-Lindström, S., Berge, J., Westrin, Å., Öjehagen, A. & Pavulans, K. S. Long-term risk factors for suicide in suicide attempters examined at a medical emergency in patient unit: results from a 32-year follow-up study. BMJ Open 10, e038794 (2020).
CP-312087